Photo source: www.sfari.org
*Recommended Reading:
My FBA post
A Work in Progress by Ron Leaf & John McEachin
The world of ABA therapy basically has two main areas of focus: Skill Acquisition, and Behavior Reduction. In a nutshell, skill acquisition is about increasing or adding appropriate skills such as attending, task completion, or following instructions.
Behavior reduction is about decreasing or extinguishing behaviors that interfere with learning or functioning, such as tantrumming, aggression, or elopement (wandering/running away).
Firstly, when beginning ABA therapy I have observed that people often want to just focus on skill acquisition. Parents request that their child learn to use utensils, get toilet trained, or learn to play appropriately with toys. Problem behaviors often are thought of as “we’ll work on that later”, or “there’s nothing that can be done about that”. Allow me to debunk these inaccurate beliefs.
It is critical in
order to effectively teach skills, that disruptive behaviors are dealt with. It
is also critical in order to enter less restrictive learning environments that
disruptive behaviors are addressed.
I was just telling a consultation client about a week ago, that her son’s behavioral issues will put him in a more restrictive support category than his cognitive level would suggest. In other words, his behaviors would place him in special education when intellectually, he is capable of grade level work. That is how detrimental problem behaviors can be. People often think it is the skill deficits that will lead a child with special needs to be placed in more restrictive settings. I would disagree. It is usually when the child is disruptive or aggressive, runs out of the room, or tantrums, that people quickly want to shuttle them into a more restrictive setting. It’s the behaviors that are likely to limit the child’s options, not their diagnosis/disability.
It isn’t uncommon, whether with parents or professionals, that people get plain ol’ freaked out about problem behaviors. When working with new staff, I often notice that when problem behaviors starts the staff will unconsciously start breathing faster, back away from the client, or their eyes will get very wide.
What is so great about ABA therapy, is there are more options to manage behavior than I can even type out in this blog post. You never have to feel hopeless or helpless about managing problem behavior. Isn’t that great news??
So now that you know it is not in your or the child’s best interest to avoid or postpone dealing with problem behavior, and that you have TONS of options to do so, let’s look at some of those options.
But first, read the disclaimer:
“It is not possible within this post to provide specific behavior reduction strategies that will be effective for every individual, or for every behavioral problem. ABA therapy is not a cookie cutter approach, nor is it one size fits all. These helpful tips do not replace the need for a Functional Analysis of disruptive behaviors, conducted by an individual credentialed to perform such tasks”
BEHAVIOR MANAGEMENT TIPS
-
During intake/assessment,
beyond just determining what skills to teach it is imperative to look at what
behaviors to target for decrease. If the client has never received intervention
services before, there are likely multiple disruptive behaviors that need to be
addressed. It’s best to select the 2-4 highest priority behaviors, because it
will be hard on the staff, the family, and the client, to try and tackle everything
at once. Quick tip: select the behaviors that interfere with teaching, or are
harmful to self or others FIRST.
-
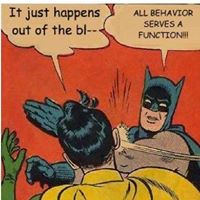
A Functional
Analysis and/or Assessment of the target behaviors must be completed, in order
to understand WHY the client is engaging in the behaviors. Do not skip this
step. It is really, really important.
-
Once the
function of the target behavior(s) has been determined, a Behavior Intervention
Plan must be created. The plan should include both preventative and reactive
strategies for reducing the target behavior(s), as well as replacement
behaviors/skills. For example, if my client pushes peers on the playground when
they get too close to him, this tells me my client needs instruction in both
social interaction as well as a method to communicate to replace aggression.
-
When the
Behavior Plan is complete, ALL relevant caregivers must be trained on it. This
includes parents, the nanny/babysitter, the ABA team, the teacher, etc. Whoever
you do not train on the Behavior Plan, you are basically saying “You’re on your
own….good luck!”
-
Data
collection is essential. How will you know if the Behavior Plan is effective if
you are not collecting data on the target behavior(s)? Regardless of how super-
duper smart you may be, all of us have created Behavior Plans that just weren’t
as effective in reducing the target behavior(s) as we thought they would be. It
happens.
-
Be sure to
set realistic behavior reduction goals. If the client is tantrumming 5-10 times
per day when services begin, it would be ridiculous to set a goal of completely
extinguishing tantrumming within 4 weeks. Be realistic. It took time for the
client to learn the behavior, it will take time for them to “un-learn” the
behavior.
Lastly, it is important to understand (and pursue additional training or expertise in) the art of de-escalation. If you are an ABA professional and work with aggressive/severe behavior clients, your employer should provide some type of physical management training to you.
De-escalation is a process through which you learn to identify when the client is becoming agitated, and you then begin to change your behavior to bring them back down to their optimal behavioral state. Instead of waiting for full explosion to occur, any step toward fully escalated would prompt a quick reaction. I have seen this method work quickly and effectively to defuse a potentially violent/dangerous situation.
Sadly, this technique is the exact opposite of what most parents and
professionals naturally do. When a child begins to yell or curse, it seems
common sense to go TOWARDS the child or to speak LOUDER to the child, but in a
proper de-escalation model those actions are both no-no’s. I also love
de-escalation techniques because eventually the client can learn to independently
calm themselves down, which should always be the optimal goal.







No comments