Photo source: www.traditionoflondonshop.com, broedor10.wordpress.com
In the military, the frontline are the first ones to go into the heat of the battle.
For preschool age children, they are usually spending all day at home with parents or at a daycare/preschool. Due to the age of children served, day care staff (and related professionals) tend to work with many special needs children--whether they realize it or not.
Not all needs are "visible", especially for children under the age of 3. A diagnosis at that age may just look like persistent, daily behavioral challenges.
The parents are not always the first recognize signs of Autism....sometimes it isn't until the child is placed in a group of their peers, or a structured setting, that deficits and impairments become obvious.
For many of my clients, it was through a bad experience with a day care or preschool that the diagnosis process began. The child was kicked out of a day care (or multiple day cares), or the parent was constantly called about behaviors issues. I often hear one of two complaints: "That super expensive and upscale preschool wouldn't let my child stay because of his behaviors" or "That super affordable and welcoming preschool had NO idea how to handle my child's behavior".
Just like I have a helpful Top 10 list for parents who are seeing issues/problems at home but don't have the benefit of a team of therapists, I think its important to have a similar list of tips for day care workers.
Please share this information with anyone who could benefit from it, as I strongly believe that highly trained day care workers can be KEY in early diagnosis and early treatment. I mean, they're the frontline staff! They need proper training and support to perform their job, and they need to be trained on Developmental Delays in order to clearly communicate any indicators to parents and caregivers.
The parents are not always the first recognize signs of Autism....sometimes it isn't until the child is placed in a group of their peers, or a structured setting, that deficits and impairments become obvious.
For many of my clients, it was through a bad experience with a day care or preschool that the diagnosis process began. The child was kicked out of a day care (or multiple day cares), or the parent was constantly called about behaviors issues. I often hear one of two complaints: "That super expensive and upscale preschool wouldn't let my child stay because of his behaviors" or "That super affordable and welcoming preschool had NO idea how to handle my child's behavior".
Just like I have a helpful Top 10 list for parents who are seeing issues/problems at home but don't have the benefit of a team of therapists, I think its important to have a similar list of tips for day care workers.
Please share this information with anyone who could benefit from it, as I strongly believe that highly trained day care workers can be KEY in early diagnosis and early treatment. I mean, they're the frontline staff! They need proper training and support to perform their job, and they need to be trained on Developmental Delays in order to clearly communicate any indicators to parents and caregivers.
Tips for Frontline Staff
- Screening Tools - The very first thing a day care or preschool should look at improving is the intake process for enrolling a child. I have worked in preschools, so I know that often this process is basically a quick interview and completing a few forms. This just isn't thorough enough. Proper intake needs to gather family background, include observation of the child/interaction with the child, ask about developmental milestones, determine child strengths and deficits, and I recommend including a brief screening. Screening tools are intentionally easy to administer, quick, and can be administered by pediatric/healthcare providers. I am not saying diagnose every child that comes through the door of the day care. Screenings are about catching red flags, not diagnosing. With the information gained from a screening checklist, the day care provider can now alert the parent to seek further evaluation, modify instruction, and be prepared that there may be behavioral challenges. Here is a great link for various screening tools.
- Amp up the structure - Typical day care classrooms have a schedule that is followed and taught to the children. For young children with Autism, this may need to be much more concrete and visible. I suggest a visual schedule clearly posted in the classroom, along with "schedule checks" throughout the day where the children are reminded what is coming next as well as "transition warnings", where the children are given verbal reminders that an activity is ending. What workers may notice is that unstructured times or days (such as a party the last day before a long break) are the WORST behavioral days for some of the children. This is likely due to an unwanted or confusing change in schedule/consistency, from the perspective of the child.
- Toss chronological age out the window - Conducting proper intake will help to determine a child's developmental age, but its important that day care workers understand that just because a child is "4" that may not mean anything. That child may not communicate, eat, play, or use a toilet like a typical 4 year old. So if the child is 4 with a developmental age of 18 months, some decisions will have to be made about placement. What classroom is best suited for this child? Will staff toilet train the child? Are there enough staff in the classroom to help the child perform self help tasks (such as eating lunch)? How will staff communicate with the child?
- Incorporate multi-sensory experiences - The preschools I have worked with always had a "sensory area" of the room, such as a popcorn tub, water table, clay table, tactile wall, etc. Usually the workers will observe that certain children gravitate to these areas, all throughout the day......they just seem to want lots of time to manipulate these objects. In addition to an area of the room, I suggest adding a sensory component to teaching times (this will keep you from constantly pulling Edward away from the tactile wall). During Circle Time, make sure the children have objects to hold, shake, or bounce. On the playground, use trampolines, swings, or huge yoga balls.
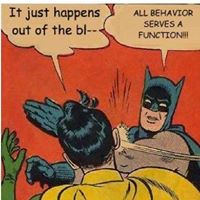
- Function based behavior management - This is SO important!!! The #1 reason I get called in to day cares or preschool settings is problem behavior. Almost without exception, when I go in to observe what I see is that everyone around that child is reinforcing the problem behavior. The child runs around the room during Circle Time, so they get sent to the Directors office. The child screams during nap time, so the teacher lies down on their mat with them. The child refuses to share toys from home, so the other children are told to not touch their toys. It is important to take a good look at the current behavior management system used at the day care, and evaluate its effectiveness. Be knowledgeable about the FBA process, as well as proactive behavior strategies that prevent behavioral blow ups in the first place. Daycares: train your staff so they know how to address challenging behaviors!
- Don't be afraid to call in the Calvary - Do not be hesitant to seek outside help when needed. For the parents, did you know most day cares set aside funds for outside trainings or consultations with professionals? For the day cares, did you know you can work with contract BCBA's both locally and remotely? A typical day care won't have Autism or behavior experts on staff. So consider working with local professionals to create trainings, put together workshops for staff, or as a part time Consultant.
- Expect to deal with this - As I already said, whether preschools/day cares are aware or not, there are likely already multiple children present on the Spectrum (or with other developmental delays). When a child is that young, it is very likely they don't have a diagnosis yet. Even if the parents have noticed concerning symptoms, they might not know the seriousness of what they are seeing. Or, there's always denial....denial is very real. So my last tip to day care workers is approach your classroom each day with a watchful, intentional eye, and be on the lookout for red flags in the children you serve. You can help point a parent towards much needed professional help. Also, please clearly state limits of competency to the families you serve. I have worked with multiple families who were told by XYZ daycare "Oh we have staff trained to work with Autistic kids, your child will do just fine here!".....cut to a few weeks later and my client has been kicked out of the daycare. :-( If the facility/day care is not properly trained or set up to serve kids with behavior issues or delays in language, toileting, self-help skills, etc., clearly explain that to parents (refer out) or seek out a professional to help the staff get trained (equip the team).
*Recommended Resources:
Lushin V, Marcus S, Gaston D, et al. The role of staffing and classroom characteristics on preschool teachers’ use of one-to-one intervention with children with autism. Autism. 2020;24(8)