Photo source: www.hamermetalart.com, www.393communications.com
What’s “NR” you ask? A common way to collect data after a
trial in which the learner not only did not give a correct response, but didn’t
respond at all, is to score “no response” (NR).
While motor actions can be prompted if the learner does not
do anything, vocal responses cannot. I say to my staff all the time, “we can’t
reach into his/her throat and pull out words”. So if you say to your client “What
color is the sun? YELLOW” and they just stare at you, then that was a “no
response” trial.
I can
absolutely relate to how it feels to bring your A-game, put on your animated
face, and get a lot of nothing in return. It’s frustrating, and makes you doubt
your clinical skills.
When correct responding disappears from the session, some
clients may turn super silly and distracted, or some may have a spike in
aggression. Just between you and me, I would much rather deal with one of those
scenarios. It’s the completely non-responsive individual that I find to be the
most challenging…..it is kind of like your clients body remained in the chair,
but the rest of them got up, walked out of the building, and is headed somewhere
FAR more exciting.
Here are a few
things that definitely do not work, are ineffective, and should be avoided:
· *Waiting the client out – I have seen a few
therapists try this one, and usually the client is perfectly content to keep
staring into space as you wait them out. And lets be real, your session is only so long. The client is quite aware that you will tire of this game before they do :-)
· *
Continue teaching/Keep up the status quo – Think
of it like this, if your client has completely stopped any correct responding
and you just keep plugging away: Is learning happening?
· *
Speak louder – Sound silly? I see it a lot.
· *
“Saaaam…..Sam!....Helloooooo, Sam?” – If your
client is not responding to task demands or any of your instructions, odds are
they also will not respond to their name being called.
Now that we got all the stuff that does not work out of the
way, I really only have one suggestion for what you SHOULD try when those NR blues kick in. It may be just one suggestion, but it can look about
900 different ways depending on the learner.
Change
something about YOU.
What my staff usually say to me (and how I used to look at
this back in the day) is: “I tried this,
and that, and this, and Sam just won’t attend/listen/respond! I don’t know what
else to do to get him to (insert whatever response the therapist is expecting)”.
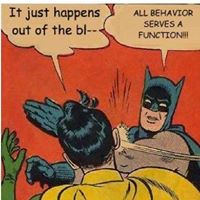
What I am suggesting, is flip that statement on its head and
instead ask yourself: “What can I do
differently that will motivate Sam to respond? Am I interesting? Am I
reinforcing? Would I want to attend to me? Is this program interesting? Are
these materials engaging? When did I last reinforce any of his behavior? Is my frustration/annoyance
showing on my face? Does my voice sound irritated? Am I moving through targets
too quickly? Too slowly? How can I be more fun?”.
See the difference? Instead of unintentionally blaming Sam for his lack of responding, first blame
yourself. Then, look at your options and start trying them out to see what is
effective. I am a big fan of “Let’s try
this and see what happens”. Even if you try something and it fails, you just
learned 1 thing that does NOT work. Which is still progress.
** Recommended Reading: